Cracking The Code Into Diabetes
Friday, November 09, 2018
When Aleksi was diagnosed with type 1 diabetes at age 9, he was automatically put on insulin treatment. “We have never slept a night since,” says his father, Nikolas. “Both my wife and I need to get up at night to check his blood sugar levels.” Levels too low could send Aleksi into a coma, and those too high will have dramatic long-term impacts on his heart, kidneys, even his extremities.
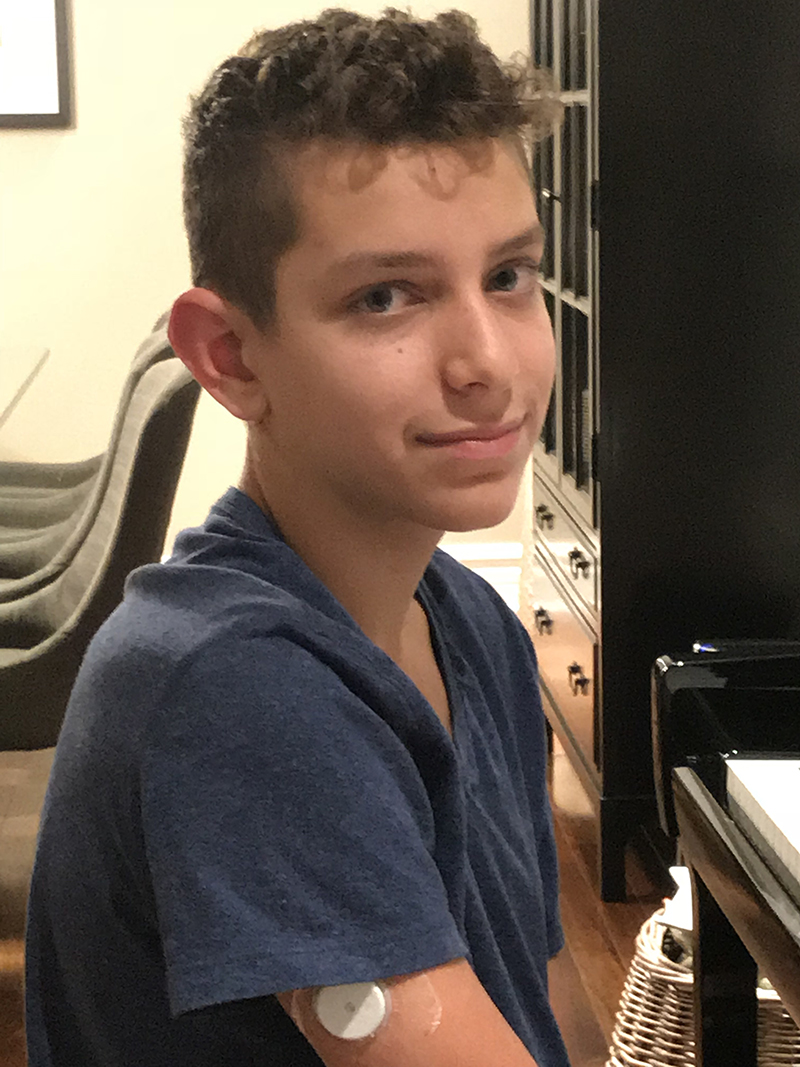 Aleksi, 13, tries to lead a normal life, but he must inject insulin
into his body 4 to 6 times a day, at school, or before an activity,
or after eating. “He’s become a human calculator of blood sugar
levels to understand what affects his body.”
Aleksi, 13, tries to lead a normal life, but he must inject insulin
into his body 4 to 6 times a day, at school, or before an activity,
or after eating. “He’s become a human calculator of blood sugar
levels to understand what affects his body.”
It doesn’t always have to be that way.
Dr. Constantin Polychronakos, Pediatric Endocrinologist at the Children’s and Senior Scientist at the Research Institute of the MUHC is doing research that has the potential of allowing thousands of children and teenagers to benefit from less invasive treatments, like taking a pill, for their particular condition.
“Through genetic testing, we have seen that a very small proportion of type 1 patients have other forms of diabetes that can be treated with alternatives to insulin,” says Dr. Polychronakos, who firmly believes this proportion could be much higher.
With help from donors, like HSBC Bank Canada, Dr. Polychronakos, wants to lead a Canada-wide study to test a list of candidate genes as well as the known genes, on 6,000 type 1 diabetic children from 19 participating clinics. The goal? Pinpoint those who can be switched to pills. The ultimate goal? Find new ways of predicting and preventing type 1 diabetes.
Aleksi’s father supports this research. “If I can help Dr. Polychronakos open up the Pandora’s box to find out what triggers type 1 diabetes, I will be able to help families, and just knowing that is enough to support his work.”